Everything You Need to Know About a Pelvic Stress Fracture
What is a Pelvic Stress Fracture?
A pelvic stress fracture is when there’s a small crack in one of the pelvic bones caused by repetitive stress or overuse, not from a major fall or trauma. It typically develops slowly and causes deep aching pain in the groin, hip, or pelvis, especially during exercise.
An analogy…
Think of the pelvis like a bridge that carries a lot of weight and movement. If you keep loading it over and over without enough rest, tiny cracks can form, just like cracks in an old bridge under constant traffic.
What are other names that a pelvic stress fracture can be called?
Stress Fracture of the Pelvis, Pubic Ramus Stress Fracture, Pubic Bone Stress Fracture, Ischial Stress Fracture
What causes a pelvic stress fracture?
The pelvis is made up of several bones that support weight bearing, walking, running, and twisting. When bones are exposed to repeated force without enough recovery, the bone’s natural healing can’t keep up, leading to a tiny crack or fracture. Stress fractures usually occur in weight-bearing parts of the pelvis like the pubic ramus or iliac bone.
What are the signs and symptoms of a pelvic stress fracture?
- Deep, aching groin, buttock, hip, or pelvic pain
- Pain that worsens with activity, especially running, jumping, or walking long distances
- Pain that improves with rest
- Tenderness over the affected area of the pelvis
- Stiffness and difficulty moving, especially after exercise
- Limping in more severe cases
What tests are used to diagnose a pelvic stress fracture?
Palpation: Tenderness when pressing over specific areas of the pelvis
Single-leg hop test: Often painful and difficult if a stress fracture is present.
How long does a pelvic stress fracture take to heal?
Mild stress fractures (caught early) may heal in 6 to 8 weeks. More developed fractures may require 10 to 12 weeks or longer. Full return to high-impact sport may take 3 to 4 months to allow bone to fully heal and regain strength.
How does a pelvic stress fracture happen?
- Repetitive high-impact activities like long-distance running, gymnastics, or football
- Sudden increase in training volume or intensity without proper progression
- Poor nutrition, particularly low calcium or Vitamin D
- Biomechanical issues like poor hip strength or foot posture problems
- Osteoporosis or low bone density
- Poor footwear or hard running surfaces
What treatment can help a pelvic stress fracture?
- Complete rest or very modified weight-bearing depending on the severity
- Crutches or a walking aid may be needed early on to unload the fracture
- Ice therapy for pain management early on
- Rehab exercises to strengthen the hips, glutes, and core without overloading the pelvis
- Nutrition support – ensuring enough calcium, Vitamin D, and total energy intake
- Biomechanics assessment – correcting running technique, gait, or muscle imbalances
What exercises or stretches can I do for a pelvic stress fracture?
- Gentle glute and core activation exercises
- Balance training on both legs
- Pelvic stability drills
- Gradual walking progression
- Low-impact cross-training like swimming or cycling
What products can help with a pelvic stress fracture?
4 point kneeling – hip extension to abduction (Fire Hydrants)
Start on your hands and knees with your hands under your shoulders and knees under your hips.
Begin arching your back by pushing your tail bone out, making a dish with your spine.
Then, round your back by tucking your tail bone in.
Find the mid-position and keep your back straight by gently tightening your pelvic floor and deep abdominal muscles, pulling your belly button in towards your spine.
Leading with your heel, lift one leg up behind you, keeping your knee at 90 degrees.
Think about pushing the sole of your elevated foot up towards the ceiling.
Extend as far as able ensuring you do not arch your back or twist your hips as you do this.
Next, bring your knee to the outside, ensuring your foot stays aligned with your hip.
Hold this position.
Control the movement as you bring your knee back down towards the floor, then repeat.
Side lying hip abduction leg circles
Lie on your side with your bottom knee bent and your top leg straight.
Tighten your pelvic floor and lower stomach muscles.
Lift your top leg up into the air until it is inline with your upper body.
Slowly rotate the top leg round in a clockwise direction in small circles and then anticlockwise.
Plank
Lie on your front with your toes on the floor.
Place your forearms on the floor and push up, lifting your torso and legs.
Hold a straight line from your shoulders to your feet for as long as you can, preventing the back from sagging.
Keep your buttocks squeezed and your hips level.
You will feel the core muscles working.
Side plank, feet stacked
Lie on your side with your forearm on the floor and elbow under your shoulder.
Keep your legs straight and stack your feet one onto of the other.
Lift yourself up into a plank on your elbow, with a straight line from your head to your feet.
Look straight ahead, making sure your body does not roll and hips do not sag.
STOP GUESSING – START MOVING
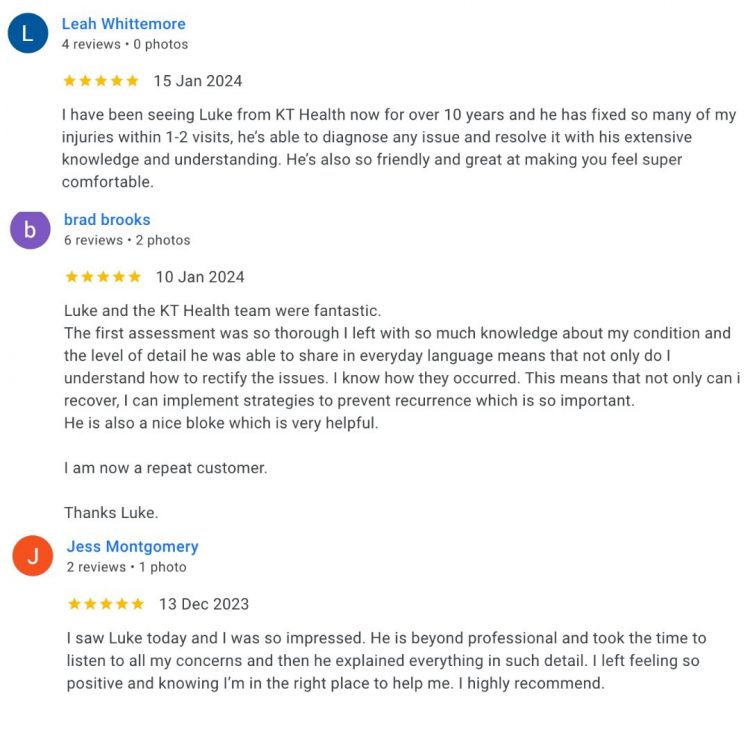
See what other people have said about our osteopaths
Trustindex verifies that the original source of the review is Google. KT health has really helped my back and i have been able to get back into competitive sportTrustindex verifies that the original source of the review is Google. Absolutely amazing, I see Louie Nouh who always listens and caters to my needs. He is amazing at his job and always helps alleviate my pain. I highly recommend Louie.Trustindex verifies that the original source of the review is Google. Friendly, supportive staff. Such a lovely place to exercise! Highly recommend.Trustindex verifies that the original source of the review is Google. Amazing instructor, I am new to Pilates felt very comfortable & supported.Trustindex verifies that the original source of the review is Google. I have been suffering from shoulder and neck pain for months - I saw Dr Louie Nouh a couple of time. His treatment really relived the pain. I have full range of movement now. His knowledge on exercise is fantastic.Trustindex verifies that the original source of the review is Google. Absolutely love reformer at menai. Instructors are amazing. Love Michaela and love the small classes. Highly recommend!Trustindex verifies that the original source of the review is Google. The trainers are all amazing , they explain everthing step by step and help where needed . It is an amazing place to relax get to know other people have a laugh . I recommend for anyone .Trustindex verifies that the original source of the review is Google. Ever since I came here I’ve been looked after by Louie and my shoulder is already feeling much better. Highly Recommend these are good people.Trustindex verifies that the original source of the review is Google. SENSATIONAL Chiropractor in Menai! I attended my first appointment with Dr Louis Nouh at KT Health & Wellness who is an absolute genius even after one session with him. He explained everything he intended to address about my lower back condition, all in easy to understand, layman’s terms. He said he would call me the next day to follow and see how I was feeling after our session and guess what, he did! During our session, he made me feel relaxed and comfortable especially as it was my first chiropractic appointment EVER! For some reason, I am actually looking forward to my subsequent sessions with him next week. Don’t get me wrong, he did poke, prod and crack me as necessary but the results made it seem worth it.Trustindex verifies that the original source of the review is Google. I have been seeing Melinda now for a couple of months to help with bursitis in my hip. She is one of the best practitioners I’ve ever seen.. With the use of various tools and techniques she has helped me recover much quicker than I expected. Thanks Mel and see you tomorrow!
We don't offer magic fixes or cures, but a sustainable approach to back pain.
Our Osteopaths will offer you a road map to help you take control of your back pain and feel great again.
BOOK YOUR OSTEOPATH VISIT TODAY
Book a Time with Dr Luke Madden Below
Book a Time with Dr Melinda Madden Below
Already have an account?
Book as a guest
- Book an Appointment